We’re pleased to announce that Pain Physicians of Wisconsin is now Pro Spine Pain.
We’re pleased to announce that Pain Physicians of Wisconsin is now Pro Spine Pain.
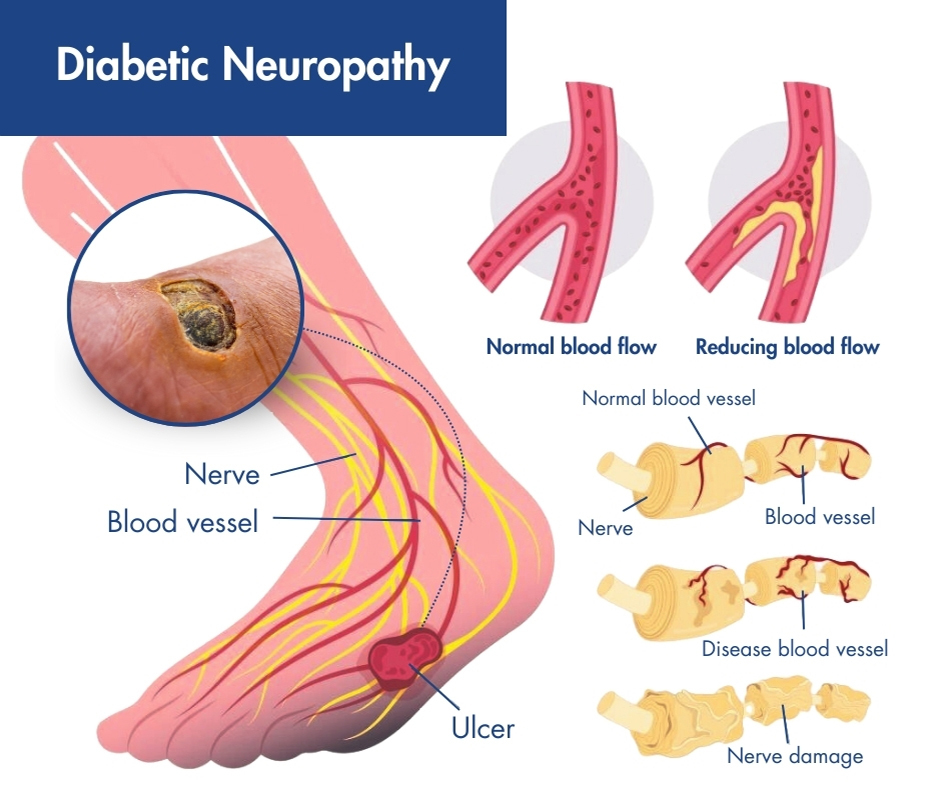 Diabetic neuropathy is a type of nerve pain that occurs as a result of diabetes, posing a significant health concern. Elevated blood sugar levels have the potential to inflict damage on nerves throughout the body by affecting the small blood vessels that supply them. Symptoms of diabetic neuropathy commonly affect the extremities, particularly the feet and legs. Seeking medical attention from the dedicated team at Pro Spine & Pain is essential to treat the painful side effects of this condition.
Diabetic neuropathy is a type of nerve pain that occurs as a result of diabetes, posing a significant health concern. Elevated blood sugar levels have the potential to inflict damage on nerves throughout the body by affecting the small blood vessels that supply them. Symptoms of diabetic neuropathy commonly affect the extremities, particularly the feet and legs. Seeking medical attention from the dedicated team at Pro Spine & Pain is essential to treat the painful side effects of this condition.
Diabetic neuropathy exemplifies the importance of diligent monitoring and control of blood sugar levels, as this can slow down or, in some cases, prevent the onset of neuropathic symptoms. Embracing a healthy lifestyle, including a balanced diet and regular exercise, is paramount for maintaining optimal limb function, reducing the risk of diabetes, and enhancing overall quality of life.
There are four main types of diabetic neuropathy: peripheral neuropathy, autonomic neuropathy, radiculoplexus neuropathy, and mononeuropathy. You can have one or more than one type of neuropathy. Your symptoms will depend on the type you have and which nerves are affected. Usually, symptoms develop gradually. You may not notice anything wrong until considerable nerve damage has occurred.
Symptoms of diabetic neuropathy can range from pain and numbness in your legs and feet to problems with your digestive system, urinary tract, blood vessels and heart. Some people experience mild symptoms, but for others, diabetic neuropathy can be quite painful and disabling.
The exact cause likely differs for each type of neuropathy. Researchers think that over time, uncontrolled high blood sugar damages nerves and interferes with their ability to send signals, leading to diabetic neuropathy. High blood sugar also weakens the walls of the small blood vessels (capillaries) that supply the nerves with oxygen and nutrients.
However, a combination of factors may lead to nerve damage, including:
Complications of diabetic neuropathy often resemble the symptoms of peripheral neuralgia and it presents a range of challenges.
Adding to the complexity of diagnosis and treatment, there are four primary types of diabetic neuropathy:
Less common is focal neuropathy, which manifests as damage to an individual nerve, commonly occurring in areas such as the hand, head, torso, or leg.
It’s possible to experience one or multiple types concurrently, each manifesting distinctively. Consequently, this single condition can generate a wide spectrum of symptoms. Given the many different potential manifestations of this condition, an accurate diagnosis by your pain management specialist in Wisconsin is essential. One of our experts will conduct several tests to determine the type of neuropathy you suffer from. This comprehensive approach ensures targeted and effective management tailored to your specific condition and symptoms.
Peripheral neuropathy is the most common type of diabetic neuropathy. It is closely linked with diabetic neuropathy and causes significant discomfort for affected individuals, primarily targeting the nerves in the feet and legs initially. Leaving peripheral neuropathy untreated increases the risk that it will spread to the arms, hands, or feet.
Symptoms of peripheral neuropathy include:
These symptoms may worsen at night, disrupting sleep with intense numbness, burning, and tingling sensations. Seeking prompt intervention is crucial to manage the condition and ensure it doesn’t progress. If you’re searching for chronic pain management specialists nearby, look no further than Pro Spine & Pain for comprehensive care and relief. Find us at one of five convenient locations in Kenosha, Waukesha, Layton, Franklin, and Madison.
Radiculoplexus neuropathy is more prevalent among individuals with Type 2 diabetes, particularly affecting older adults. This neuropathic condition targets the nerves that control activity in the hips, buttocks, thighs, and legs, often inducing severe pain that is frequently misidentified as sciatica.
Unexplained weight loss may serve as an early indicator of radiculoplexus neuropathy, while certain cases can also lead to abdominal swelling. Difficulty in rising from a seated position may signal muscle weakness due to atrophy in the thighs, a potential sign of neuropathic involvement. Recognizing these symptoms is crucial for timely diagnosis and management of radiculoplexus neuropathy.
Autonomic neuropathy is a condition affecting the nervous system governing involuntary bodily responses, like digestion, perspiration, or the activity of the heart and other organs. Unlike voluntary actions, such as moving a limb, you don’t consciously command your heart to beat; it functions automatically. The extensive network of your nervous system interconnects every part of your body, making the symptoms of autonomic neuropathy wide-ranging and complex.
Due to the multifaceted nature of this condition, for an accurate diagnosis, it’s imperative to seek assessment at a leading pain management clinic in Wisconsin. Symptoms encompass heightened risks of hypoglycemia from failure to regulate high blood sugar, urinary bladder complications ranging from infections to retention or incontinence, gastrointestinal disturbances like diarrhea or constipation, increased sensitivity, difficulty swallowing, altered responsiveness of the eyes to light, drops in blood pressure, and diminished sexual response, manifested by issues such as vaginal dryness and erectile dysfunction. Prompt identification and comprehensive management of these symptoms will enable you to address autonomic neuropathy and enhance your overall well-being.
Mononeuropathy involves the specific impairment of a facial, leg, or abdominal nerve. Although more frequently seen among older adults, this painful form of neuropathy typically does not cause long-term effects. Symptoms associated with mononeuropathy often resolve swiftly, even without intervention, with pain typically localized to areas such as the foot, shin, thigh, chest, or abdomen.
Notably, mononeuropathy may also impact the function of the eyes, presenting symptoms like eye pain, episodes of double vision, or difficulty focusing. If you have episodes of eye symptoms, seek evaluation at one of Wisconsin’s premier pain clinics. Pro Spine & Pain have locations in Kenosha, Waukesha, Layton, Franklin, and Madison. Left untreated, mononeuropathy carries the risk of complications like facial paralysis, such as Bell’s palsy, underscoring the importance of prompt diagnosis and management.
Treatment for diabetic neuropathy is tailored to the specific type of neuropathy you have and the types of nerve damage. Our top pain management specialists offer a range of diagnostic tests to accurately assess your condition. These may include nerve studies, sensory testing, autonomic testing, electromyography (EMG), and filament testing, which measures touch sensitivity.
For those experiencing chronic pain from the symptoms of diabetic neuropathy, peripheral nerve stimulation can be a valuable intervention. Using electrical pulses, this therapy disrupts pain signals, potentially reducing the need for pain medications.
While diabetic neuropathy cannot be cured, its progression can be slowed, and discomfort effectively managed. Keeping blood sugar levels within a healthy range is crucial for people with diabetes. Despite the challenges posed by severe diabetes, it is possible to lead a fulfilling and comfortable life. Partnering with a reputable pain management clinic can provide the support and interventions needed to achieve this goal. Don’t hesitate to contact Pro Spine & Pain today to start your journey toward improved quality of life.
Thomas Stauss, MD, completed both his undergraduate and medical studies at the esteemed University of Wisconsin in Madison. Dr. Stauss values having access to a wide array of cutting-edge treatment options, ensuring effective relief for his patients' discomfort and a significant enhancement in their quality of life. More specifically, he specializes in utilizing implanted devices to manage chronic pain. Dr. Stauss’s primary objective is to uphold the dignity of each patient while delivering ethical and professional services.
More about Dr. Stauss